The blood components
Author: Maria Yiallouros, erstellt am: 2017/03/01, Editor: Maria Yiallouros, English Translation: PD Dr. med. Gesche Tallen, Last modification: 2017/03/01
Table of contents
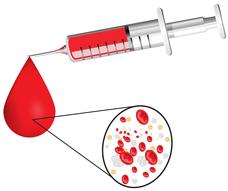
About 60 % of the body’s total blood volume is made by blood plasma, a yellowish liquid that contains mostly water, but also different proteins, minerals and vitamins. About 40 % of the blood volume is made by blood cells of the following three different types, which present in different fractions and fulfilling different tasks:
- red blood cells (erythrocytes)
- white blood cells (leukocytes)
- platelets (thrombocytes).
Red blood cells (erythrocytes)
The red blood cells, also known as erythrocytes, comprise about 99 % of all circulating blood cells. One microliter (one millionth of a liter) of blood contains four to six million erythrocytes.
The most important function of the red blood cells is oxygen supply. They contain the iron-containing transport-protein haemoglobin, which gives the blood its red colour and carries oxygen from the lungs to the body’s different organs and tissues.
Patients with a lack of red blood cells (anaemia) or impaired function due to a lack of haemoglobin (iron-deficiency anaemia), respectively, may suffer from the consequences of insufficient oxygen supply. They may present with signs of anaemia, such as pallor, fatigue, general weakness, shortness of breath, a drop in performance levels, back pain and headaches.
To find out if the red blood cells are functioning properly, the doctors primarily assess the total volume (haematokrit, Hkt) – rather than the number – of circulating erythrocytes. In addition, the concentration of haemoglobin (Hb) in the blood is measured. In healthy children older than one year, the Hb ranges between 10 and 16 g/dl and Hkt between 30 and 49 % (see table) [KUL2002].
If a child presents with signs of anaemia and Hb- and Hkt-values below the normal range, for example due to leukaemia or after a chemotherapy, a transfusion of red blood cells from a healthy donor can help stabilising the patient’s condition.
|
Age |
Haemoglobin (Hb) [g/dl] |
Haematokrit (Hk) [%] |
|---|---|---|
|
1 year |
10.1 - 13.0 |
30 - 38 |
|
2 – 6 years |
11.0 - 13.8 |
32 - 40 |
|
6 – 12 years |
11.1 - 14.7 |
32 - 43 |
|
12 – 18 years (females) |
12.1 - 15.1 |
35 - 44 |
|
12 – 18 years (males) |
12.1 - 16.6 |
35 - 49 |
White blood cells (leukocytes)
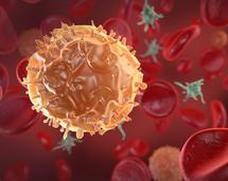
White blood cells, also known as leukocytes, represent only 1 % of all circulating blood cells. In a healthy individual, the number of white blood cells ranges between 5.000 and 8.000 per microliter of circulating blood.
White blood cells are mainly responsible for the body’s immune defence. They recognise pathogens such as bacteria, viruses or fungi and neutralise them. In patients suffering from an infection, the number of white blood cells may rapidly change, thereby providing prompt control of the germs.
Based on their shape, origin and function, there are different types of white blood cells: accounting for 60 - 70 % of all leukocytes, the granulocytes represent the largest proportion, followed by the lymphocytes with 20 - 30 % and the monocytes (which can produce macrophages, also known as „giant engulfing cells“) with 2 - 6 %.
These three different types of cells have different strategies to fight germs. Optimal infection control, however, requires close collaboration of all of them. This explains that patients with low white blood cell counts or with dysfunctional leukocytes, for example as a consequence of leukaemia, can’t fight pathogens (such as bacteria, viruses or fungi) very well, which makes them prone to infections.
The total white blood cell count (WBC), as well as the shapes of the different types of leukocytes and their percentages are determined in a patient’s blood sample (so-called differential).
Granulocytes
The granulocytes – named as those because of the small granules typically found in their cytoplasm – are mainly responsible for fighting bacteria, and, to a lesser degree, also viruses, fungi and parasites (such as worms). They make themselves promptly available after the first contact with the germ and show up with a large army at the infection site, thereby forming the first groundswell of immune response against the invader.
Granulocytes can defeat a pathogen by first embedding and then engulfing it – a mechanism called phagocytosis (ingestion). By this strategy, they also help eliminating cell debris. Last but not least, granulocytes play an important role in both allergic reactions and inflammatory processes, such as generating pus.
Acute and chronic blood cancers (leukaemias; AML, CML) arise from malignant transformations of granulocytes or their progenitor cells, respectively. In these malignancies, the number of healthy, functional granulocytes may be decreased due to the uncontrolled proliferation, thus prevalence of malignant cells.
The granulocyte count in a patient’s blood plays a major role during cancer treatment. If it decreases below 500 - 1.000 per microliter due to the cancer treatment, the patient’s risk of infection increases significantly, even including infections caused by pathogens that do not harm a healthy individual.
Lymphocytes
Lymphocytes are small white blood cells, 70% of which are found in the lymphatic tissues, such as lymph nodes, spleen, tonsils and thymus. Chains of lymph nodes localise around the mandibular angle, as well as the neck, armpits and groin, for example. The spleen is an organ in the left upper abdomen. The thymus is a small gland located behind the breastbone (sternum).
Lymphocytes are also found in the lymph, a clear fluid circulating in the lymphatic vessels, thereby forming a large vessel network in the body that is similar to the blood vessel system.
Lymphocytes have a central function within the immune system, because they can recognise, target and eliminate pathogens. They play a major role in viral infections. Lymphocytes sort of organise the job of the granulocytes and they produce so-called antibodies. These are small protein molecules that dock on to the pathogens, thereby making them recognisable for the engulfing cells (macrophages).
Lymphocytes also recognise and kill cells that have been attacked by viruses as well as cancer cells. They also make sure the body remembers those pathogens that have attacked before. Certain (immunological) laboratory tests help differentiate between several subgroups of lymphocytes, such as T- and B-lymphocytes, to name a few.
The lymphocytes in patients with acute or chronic lymphoblastic leukaemias (ALL, CLL), or their precursors, respectively, are malignantly transformed. Depending on whether B- or T-lymphocytes are affected by this malignant transformation, different subgroups of ALL and CLL exist.
Monocytes
Monocytes are a subgroup of white blood cells. They circulate in the bloodstream for a few days and then typically wander into tissues throughout the body where they differentiate into „giant engulfing cells“ or macrophages in order to engulf and, thus, eliminate, pathogens, foreign bodies and dead cells. They also present parts of the engulfed and digested organisms on their surface, thereby promoting immune response by the lymphocytes.
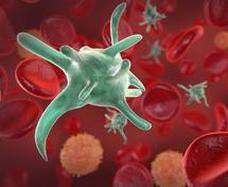
Platelets (Thrombocytes)
The platelets, also known as thrombocytes, are mainly responsible for blood clotting. They make sure that in case of a bleeding, the injured blood vessels’ walls are promptly repaired and that the bleeding stops.
Typical presenting symptoms in patients with leukaemias, such as frequent nose and gum bleeds as well as tiny, spotty bleedings into the skin (petechiae), frequent bruising, and sometimes even bleedings in inner organs are the result of low platelet counts. Chemotherapy can also lead to compromised bone marrow function, thereby decreasing platelet production.